Had he [Edward Jenner] but seriously reflected upon the specific nature of the Cow-pox virus, and endeavoured to trace the grease of the horse whence it sprang up to its origin, previously to engaging in so momentous a concern, it would have required but a small share of abilities to have predicted the dreadful consequences that have since ensued, and I am sorry to have the opportunity of showing that the result of the industry which he has shown in ingrafting an unknown disease into the human constitution, neither merits private regard, nor public approbation [approval or praise]…[1]
— Dr. Squirrel, Early 1800s
The history of the eight fatal cases I have had present, I think, peculiar points of interest. In all these vaccinations was performed. The children seemed healthy on the day of vaccination, but on the sub-sequent day Small-pox eruption appeared, the disease proceeding pari passu [step by step] with the maturation of the Small-pox vesicle. On the ninth day of the disease, with one exception, all died.”[2]
— Dr. Charteris, assistant surgeon of St Giles’ Infirmary, Lancet, July 28th, 1866
Audio in this article was partially created using ElevenLabs. With ElevenLabs, you can generate high-quality speech in any voice, style, and language. Their AI voice generator delivers incredible human-like audio that will blow your mind. Please consider clicking on the affiliate link to check them out. https://try.elevenlabs.io/1bv65kr0oz9w
The widely accepted belief is that devastating plagues once ravaged the world, only to be brought under control by medical interventions such as vaccines and antibiotics. I, too, once held this view without question—until I began examining the actual data. What I discovered was not only startling but also difficult to reconcile with everything I had been taught. The evidence challenged my deepest assumptions, forcing me to rethink the history of infectious disease and the true factors that shaped public health. It was a revelation that changed my perspective in ways I never could have imagined.
Mortality statistics in the United States began being recorded in 1900, providing a clear picture of historical disease trends. The data reveal that the vast majority of the decline in deaths occurred before the introduction of medical interventions such as penicillin and streptomycin. Whooping cough fatalities had already dropped by approximately 90% before the vaccine was introduced, while measles deaths had declined by an astonishing 98% before that vaccine’s introduction. Meanwhile, scarlet fever, which never had a widely used vaccine, saw its death rate plummet to zero, mirroring the decline of these other diseases.
A similar pattern emerges from mortality data in England and Wales, where record-keeping began 62 years earlier than in the United States, in 1838. The decline in deaths is nothing short of remarkable. Fatalities from whooping cough and diphtheria had already fallen to nearly zero before the introduction of the DTP vaccine—where "D" stands for diphtheria and "P" for pertussis, or whooping cough.
Smallpox deaths also dropped to near zero by the end of the 1900s following a century of vaccination. However, the simultaneous decline of all other major diseases raises doubts about the vaccine’s true role—a point I’ll explore further later in this article. Perhaps most striking is the case of scarlet fever, often called the "fell destroyer," which often claimed more lives than whooping cough, measles, and smallpox combined. Yet its death toll vanished entirely, without the aid of antibiotics or a vaccine, paralleling the decline of these other diseases.
When we combine the mortality rates for scarlet fever, whooping cough, measles, diphtheria, and smallpox, a striking pattern emerges—a nearly 98% decline in deaths occurred before the mass production of penicillin.
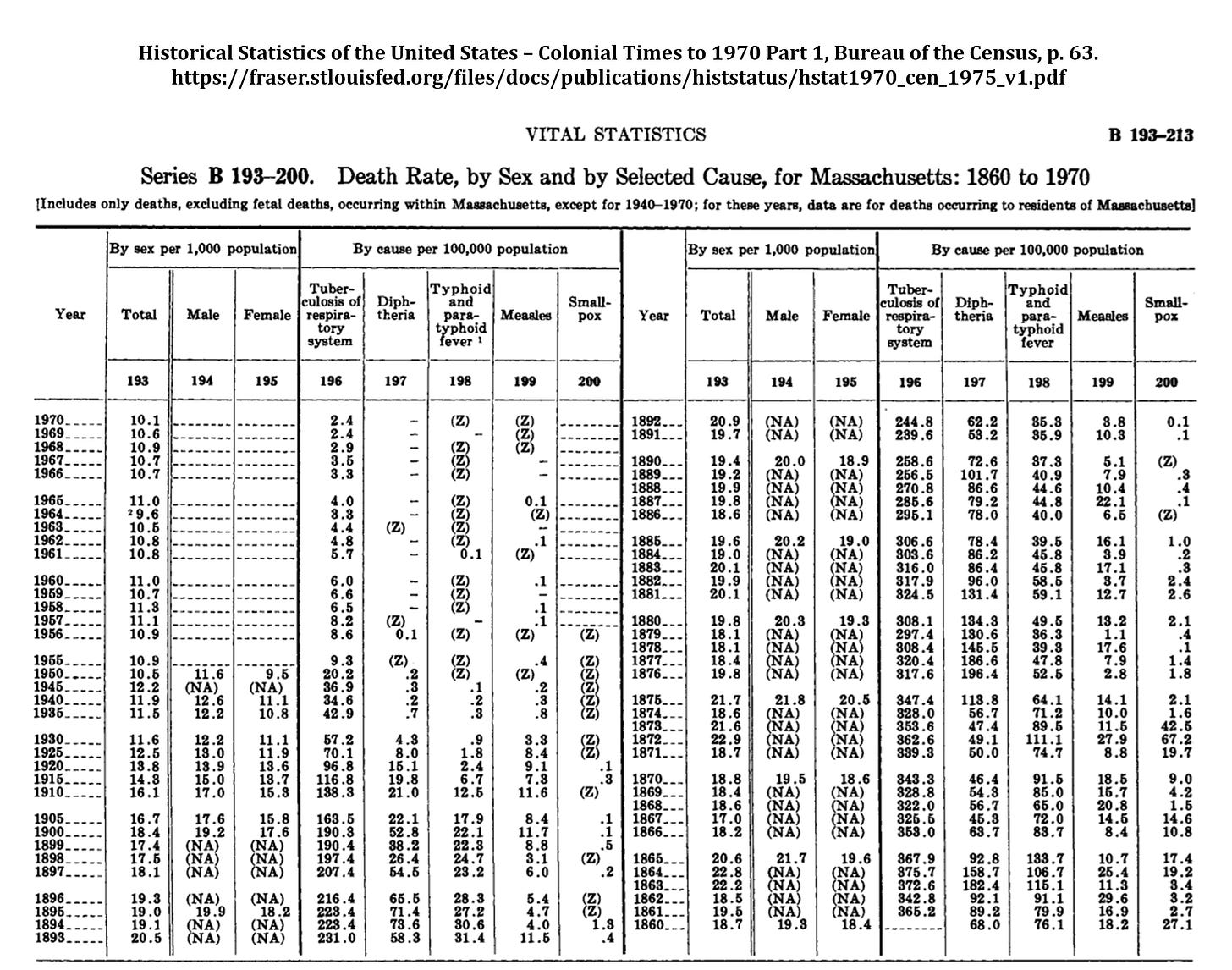
Data from Massachusetts reveals the same striking trend in the decline of infectious diseases. Once again, diphtheria had already fallen to nearly zero before the introduction of the DTP vaccine. Measles had been at or near zero for eight years before the measles vaccine was introduced in 1963. Meanwhile, typhoid and paratyphoid fever—far deadlier than measles—vanished entirely without the introduction of any vaccine.
Perhaps most astonishing are the figures on tuberculosis, historically known as consumption or the white plague. In 1861, tuberculosis killed at a rate of 365.2 per 100,000, while measles claimed 16.9 per 100,000 and smallpox just 2.7. This means tuberculosis was over 21 times deadlier than measles and more than 135 times deadlier than smallpox. Yet, despite its devastating toll, tuberculosis is rarely discussed in the same breath as other historic epidemics, likely because we do not widely vaccinate for it today. Notably, neither the introduction of the antibiotic streptomycin in 1947 nor the BCG vaccine in 1954 significantly impacted tuberculosis’s already steep downward trajectory.
Adding to this body of evidence, medical journals have, at times, acknowledged the dramatic decline in both mortality rates and the severity of these diseases. Key excerpts from these publications are presented here for your consideration, offering firsthand insights into the historical trends that challenge conventional narratives.
“In the majority of children the whole episode has been well and truly over in a week . . . In this practice measles is considered as a relatively mild and inevitable childhood ailment that is best encountered any time from 3 to 7 years of age. Over the past 10 years there have been few serious complications at any age, and all children have made complete recoveries. As a result of this reasoning no special attempts have been made at prevention even in young infants in whom the disease has not been found to be especially serious.”[3]
“…it may be questioned whether universal vaccination against pertussis is always justified, especially in view of the increasingly mild nature of the disease and of the very small mortality. I am doubtful of its merits at least in Sweden, and I imagine that the same question may arise in some other countries. We should also remember that the modern infant must receive a large number of injections and that a reduction in their number would be a manifest advantage.”[4]
“There was a continuous decline, equal in each sex, from 1937 onward. Vaccination [for whooping cough], beginning on a small scale in some places around 1948 and on a national scale in 1957, did not affect the rate of decline if it be assumed that one attack usually confers immunity, as in most major communicable diseases of childhood... With this pattern well established before 1957, there is no evidence that vaccination played a major role in the decline in incidence and mortality in the trend of events.”[5]
“In the United Kingdom and in many other countries, whooping cough (and measles) are no longer important causes of death or severe illness except in a small minority of infants who are usually otherwise disadvantaged. In these circumstances, I cannot see how it is justifiable to promote mass vaccination of children everywhere against diseases which are generally mild, which confer lasting immunity, and which most children escape or overcome easily without being vaccinated.”[6]
“Most cases of whooping cough are relatively mild. Such cases are difficult to diagnose without a high index of suspicion because doctors are unlikely to hear the characteristic cough, which may be the only symptom. Parents can be reassured that a serious outcome is unlikely. Adults also get whooping cough, especially from their children, and get the same symptoms as children.”[7]
“...nearly 90% of the decline in infectious disease mortality among US children occurred [from 1900] before 1940, when few antibiotics or vaccines were available.”[8]
“The usual explanation offered for this changed trend in infectious diseases has been the forward march of medicine in prophylaxis and therapy but, from a study of the literature, it is evident that these changes in incidence and mortality have been neither synchronous with nor proportionate to such measures. The decline in tuberculosis, for instance, began long before any special control measures, such as mass x-ray and sanitarium treatment, were instituted, even long before the infectious nature of the disease was discovered. The decline in pneumonia also began long before the use of the antibiotic drugs. Likewise, the decline in diphtheria, whooping cough and typhoid fever began fully years prior to the inception of artificial immunization and followed an almost even grade before and after the adoption of these control measures. In the case of scarlet fever, mumps, measles and rheumatic fever there has been no specific innovation in control measures, yet these also have followed the same general pattern in incidence decline. Furthermore, puerperal and infant mortality (under one year) has also shown a steady decline in keeping with that of the infectious diseases, thus obviously indicating the influence of some over-all unrecognized prophylactic factor.”[9]
“In general, medical measures (both chemotherapeutic and prophylactic) appear to have contributed little to the overall decline in mortality in the United States since about 1900—having in many instances been introduced several decades after a marked decline had already set in and having no detectable influence in most instances. More specifically, with reference to those five conditions (influenza, pneumonia, diphtheria, whooping cough, and poliomyelitis) for which the decline in mortality appears substantial after the point of intervention—and on the unlikely assumption that all of this decline is attributable to the intervention... it is estimated that at most 3.5 percent of the total decline in mortality since 1900 could be ascribed to medical measures introduced for the diseases considered here.”[10]
In their analysis, McKinlay presents a striking chart that juxtaposes the dramatic decline in mortality over the past century with the astonishing rise in healthcare costs. The contrast is undeniable: as death rates from infectious diseases plummeted, the financial burden of medical care soared.
Perhaps most startling is the sheer scale of modern healthcare expenditures. As of 2023, estimates indicate that U.S. healthcare spending reached a staggering $4.9 trillion, accounting for 17.6% of the nation's Gross Domestic Product (GDP). This upward trend shows no signs of slowing, with projections suggesting that healthcare spending could approach—or even surpass—20% of GDP by 2032.
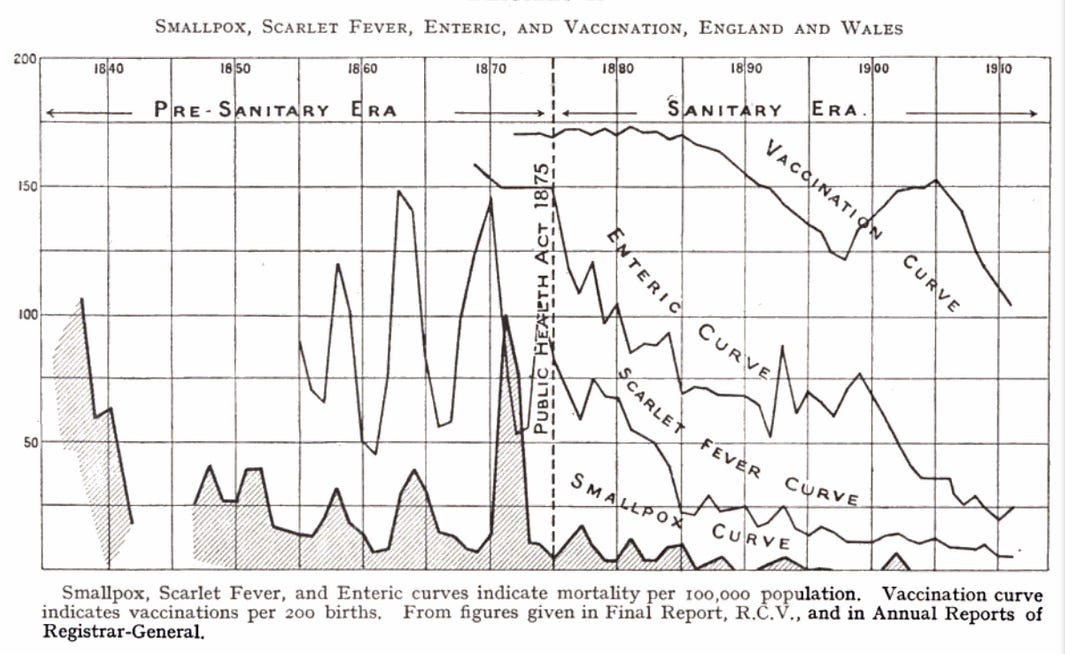
The widely held belief that smallpox was eradicated solely due to the vaccine was increasingly called into question by the late 1800s and early 1900s. In his 1914 book The Vaccination Question in the Light of Modern Experience: An Appeal for Reconsideration, Dr. C. Killick Millard highlighted the simultaneous decline in mortality rates for smallpox, scarlet fever, and enteric fever (a disease largely forgotten today). Particularly striking is that this decline in smallpox mortality coincided with a significant decrease in smallpox vaccinations being administered. Dr. Millard, observing this pattern, logically concluded that the decline in smallpox deaths was not directly caused by vaccination but other, unidentified factors.
“Moreover, it will be noticed that the drop in the mortality from ‘other zymotics’ was almost as striking. So much is this the case, that, without being informed, it is difficult to tell which line represents small-pox, and which ‘other zymotics.’ Obviously, causes other than vaccination must have been at work to have produced this fall in ‘other zymotics,’ and we cannot say that the same cause did not also influence the mortality from smallpox.”[11]
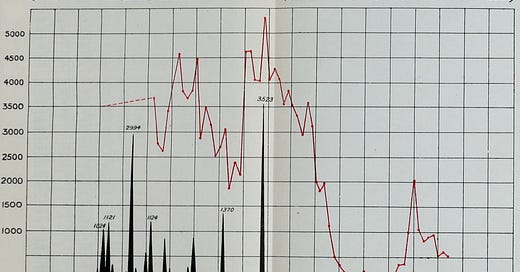
In 1912, J.T. Biggs presented a compelling analysis in his work Sanitation Versus Vaccination, including a diagram that mirrored Dr. Millard’s finding.[12] Biggs focused on Leicester, England, and showed a striking pattern: smallpox deaths decreased after a major epidemic in 1872, even though vaccination rates were high during the outbreak. However, as vaccination rates began to decline, smallpox deaths continued to decrease and remained low despite the reduced vaccination coverage.
According to prevailing medical beliefs at the time—and still held by many today—one would have expected smallpox deaths to rise as vaccination rates fell. Yet, the reality was the complete opposite, with mortality continuing to decrease regardless of vaccination efforts. This contradiction challenges the conventional narrative and suggests that other factors played a key role in reducing smallpox deaths during this period.
Historical mortality data from the United States, England & Wales, and Massachusetts reveal a striking trend: the vast majority of the decline in deaths from infectious diseases occurred before the widespread use of vaccines and antibiotics. Records show that diseases like whooping cough, measles, diphtheria, and scarlet fever had already seen dramatic reductions—some by nearly 100%—before medical interventions were introduced. Scarlet fever, a once-deadly disease, disappeared entirely without a vaccine, while tuberculosis mortality plummeted long before the introduction of the BCG vaccine or streptomycin. These patterns challenge the prevailing belief that vaccines and antibiotics were the primary drivers of improved public health.
Medical journal entries further support this perspective, with experts acknowledging the increasingly mild nature of diseases like measles and whooping cough, questioning the justification for mass vaccination, and highlighting the lack of correlation between medical interventions and mortality declines. Studies such as McKinlay’s analysis reveal that while disease-related deaths have declined, healthcare costs have skyrocketed, with U.S. expenditures in 2023 reaching $4.9 trillion and projected to consume 20% of GDP by 2032. The implications of this relentless increase raise critical questions about the efficiency, effectiveness, and sustainability of modern medical interventions.
Perhaps most strikingly, historical data also challenges the narrative around smallpox. A 1914 study by Dr. C. Killick Millard and J.T. Biggs’ 1912 work Sanitation Versus Vaccination both show that smallpox mortality rates dropped significantly, even as vaccination rates declined. In Leicester, England, smallpox deaths decreased after a large epidemic in 1872, and as vaccination rates fell, mortality remained low. This contradicts the prevailing medical belief that lower vaccination rates would lead to higher mortality, raising the question of what other factors may have contributed to the decline of smallpox.
These findings suggest that broader societal factors—such as improved sanitation, nutrition, hygiene, and living conditions—played a far more significant role in reducing infectious disease mortality than previously credited. As the cost of healthcare continues to rise, a deeper examination of the historical trends and underlying drivers of health improvements is essential for shaping future public health policies and medical practices.
[1] William Job Collins, MD, Have You Been Vaccinated, and what Protection is it Against the Small Pox? 1869, London, p. 47.
[2] William Job Collins, MD, Have You Been Vaccinated, and what Protection is it Against the Small Pox? 1869, London, pp. 37–38.
[3] Vital Statistics, British Medical Journal, February 7, 1959, p. 381.
[4] “Is Universal Vaccination Against Pertussis Always Justified?” British Medical Journal, October 22, 1960, p. 1186.
[5] “Vaccination Against Whooping-Cough: Efficacy Versus Risks,” The Lancet, January 29, 1977, pp. 236, 237.
[6] “Whooping Cough in Relation to Other Childhood Infections in 1977–9 in the United Kingdom,” Journal of Epidemiology and Community Health, vol. 35, 1981, p. 145.
[7] “Natural Course of 500 Consecutive Cases of Whooping Cough: A General Practice Population Study,” British Medical Journal, vol. 310, February 1995, p. 299.
[8] “Annual Summary of Vital Statistics: Trends in the Health of Americans During the 20th Century,” Pediatrics, December 2000, pp. 1307-1317.
[9] W. J. McCormick, MD, “Vitamin C in the Prophylaxis and the Therapy of Infectious Diseases,” Archives of Pediatrics, vol. 68, no. 1, January 1951.
[10] John B. McKinlay and Sonja M. McKinlay, “The Questionable Contribution of Medical Measures to the Decline of Mortality in the United States in the Twentieth Century,” The Milbank Memorial Fund Quarterly, Health, and Society, vol. 55, no. 3, summer 1977, p. 425.
[11] C. Killick Millard, The Vaccination Question in the Light of Modern Experience: An Appeal for Reconsideration, 1914.
[12] J. T. Biggs, JP, Sanitation Versus Vaccination, 1912, Diagram G.


















Share this post